Overview of the VLDL Lipid Test
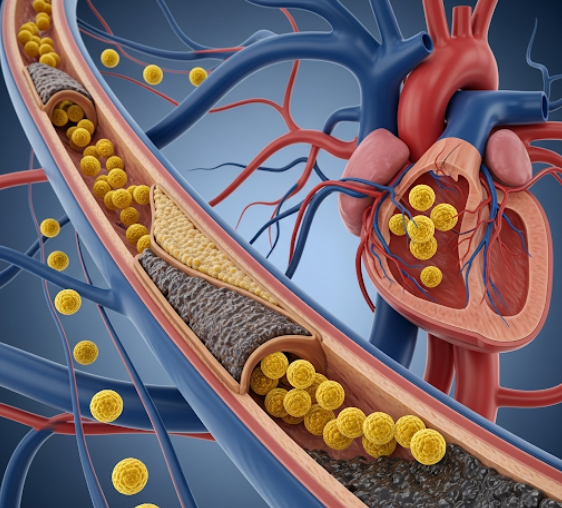
The Very Low-Density Lipoprotein (VLDL) test is a blood test that measures the levels of VLDL cholesterol in your bloodstream. VLDL is one of several types of lipoproteins, which are particles made up of cholesterol, triglycerides, and proteins. Their primary function is to transport lipids (fats) throughout the body. Among the lipoproteins, VLDL contains the highest amount of triglycerides, which are a type of fat used for energy or stored in fat cells. VLDL is produced by the liver and released into the bloodstream to deliver these triglycerides to various tissues. While VLDL is essential for the body's energy needs, high levels are considered "bad cholesterol" because they contribute to the buildup of plaque in the arteries, a process called atherosclerosis. This arterial plaque can narrow blood vessels, restrict blood flow, and significantly increase the risk of cardiovascular diseases like coronary heart disease, heart attack, and stroke. Unlike LDL and HDL, VLDL is typically not measured directly but is estimated from triglyceride levels, as approximately one-fifth of triglyceride levels usually represent VLDL.
Why the VLDL Lipid Test is Done
The VLDL lipid test is primarily performed to assess an individual's risk for cardiovascular disease. It is often included as part of a comprehensive lipid panel, which also measures total cholesterol, LDL (low-density lipoprotein), HDL (high-density lipoprotein), and triglycerides. Doctors order this test to: screen for cardiovascular disease, especially in individuals with risk factors such as high blood pressure, diabetes, obesity, a family history of heart disease, or a sedentary lifestyle. It helps in diagnosing conditions associated with abnormal lipid metabolism, particularly hypertriglyceridemia, as VLDL is rich in triglycerides. The test also assists in monitoring the effectiveness of lipid-lowering therapies, including lifestyle changes (diet and exercise) or medications. While LDL cholesterol is often the primary target for cholesterol-lowering treatments, VLDL provides additional insight into triglyceride-related cardiovascular risk. High VLDL levels are strongly linked to atherosclerosis, where fatty deposits accumulate in the arteries, making it a critical marker for evaluating overall heart health and guiding personalized treatment plans to reduce the likelihood of heart attack and stroke.
Risks
The risks associated with undergoing a VLDL lipid test are minimal, similar to those of any routine blood draw (venipuncture). These risks are typically minor, localized, and temporary. You may experience a brief, slight pain or a stinging sensation when the needle is inserted into your vein, commonly in the inner elbow or back of the hand. After the blood collection, a small bruise might form at the puncture site, which usually resolves on its own within a few days. Some individuals, particularly those who are sensitive to needles or prone to fainting, might experience transient dizziness or lightheadedness during or immediately after the blood draw. In very rare cases, a small collection of blood under the skin, known as a hematoma, might occur if bleeding continues internally at the puncture site. The risk of infection at the site of puncture is extremely low when proper sterile techniques are strictly followed by the healthcare professional performing the blood draw. While excessive bleeding is uncommon, it is a slight consideration for individuals who are taking anticoagulant (blood-thinning) medications. Overall, these potential complications are infrequent, generally mild, and do not lead to any long-term health concerns, making the VLDL test a safe diagnostic procedure.
How You Prepare
Preparing for a VLDL lipid test is crucial for ensuring accurate results, as dietary intake significantly influences lipid levels. Typically, fasting is required for 9 to 12 hours before the blood draw. This means you should not consume any food or drinks other than plain water during this period. Fasting is particularly important because VLDL levels are often estimated from triglyceride levels, and triglycerides are highly sensitive to recent food intake. It is also strongly recommended to avoid alcohol consumption for at least 24 hours prior to the test, as alcohol can significantly elevate triglyceride levels and, consequently, VLDL estimates. It is essential to inform your doctor about all medications, over-the-counter drugs, herbal remedies, and supplements you are currently taking. Certain medications, such as corticosteroids, diuretics, or even some birth control pills, can affect lipid levels. Your doctor may advise you to temporarily stop or adjust certain medications before the test, but never do so without their explicit instruction. Avoiding strenuous exercise just prior to the test can also be beneficial. Always adhere to your healthcare provider's specific instructions for the most accurate test outcome.
What You Can Expect
Before the Test
Before your VLDL lipid test, your primary step is to meticulously follow any preparatory instructions provided by your healthcare provider. This commonly includes fasting for 9 to 12 hours prior to the blood draw, allowing only plain water. It is absolutely essential to inform your doctor about all medications, supplements, and herbal remedies you are currently taking, as many can influence lipid levels. Your doctor may advise you to temporarily discontinue certain medications, but this must only be done under their direct guidance. Crucially, you should avoid alcohol consumption for at least 24 hours (or more, if instructed) before the test to ensure accurate results, as alcohol is a major factor in elevating triglyceride levels, from which VLDL is estimated. You might also be advised to avoid strenuous physical activity just before the test. On the day of your appointment, aim to arrive at the clinic or laboratory feeling relaxed and well-hydrated. If you tend to feel anxious about blood draws, informing the phlebotomist can be helpful, as they can take steps to make the process more comfortable. These preparatory steps are vital for the integrity of your test results, helping to ensure the blood sample accurately reflects your true VLDL levels for proper interpretation.
During the Test
During the VLDL lipid test, you will undergo a routine blood collection, which is a straightforward and quick procedure. You will be asked to sit comfortably, typically in a chair designed for blood draws. A trained healthcare professional, such as a phlebotomist or nurse, will identify a suitable vein, most commonly found in the crook of your arm (antecubital fossa) or, less frequently, on the back of your hand. The selected area of skin will be meticulously cleaned with an antiseptic wipe to ensure sterility and prevent any potential infection. To make the vein more prominent and easier to access, a tourniquet may be gently applied around your upper arm, which temporarily increases blood flow to the vein. Once the vein is prepared, a sterile, single-use needle will be carefully inserted. You will likely experience a brief, sharp prick or a mild stinging sensation as the needle enters the vein. Blood will then be steadily drawn into one or more small collection tubes. The actual blood collection is usually very swift, often lasting only a few minutes. After the necessary amount of blood is obtained, the tourniquet is released, and the needle is smoothly withdrawn. Pressure will then be applied to the puncture site with a cotton ball or gauze to stop any bleeding.
Results
After your blood sample for the VLDL lipid test is collected, it is promptly sent to a medical laboratory for precise analysis. Since VLDL cannot be measured directly, laboratories typically estimate its level by dividing your triglyceride level by five (when measurements are in mg/dL). This calculation is generally accurate unless your triglyceride levels are very high (e.g., above 400 mg/dL). Once the analysis is complete, a detailed report containing your estimated VLDL level, typically expressed in milligrams per deciliter (mg/dL), will be generated and transmitted to your healthcare provider, usually within a few days. Your doctor will then interpret these results in the context of established normal reference ranges. For VLDL cholesterol, a normal level is generally considered to be less than 30 mg/dL. A level of 30 mg/dL or higher is considered elevated and may indicate an increased risk for cardiovascular disease. Your doctor will discuss the findings with you, explaining what your VLDL level signifies about your cardiovascular risk, and based on these results alongside your complete medical history, other lipid panel components (total cholesterol, HDL, LDL), and any other relevant tests, they will recommend any necessary follow-up actions, such as lifestyle modifications, dietary changes, or medication to manage your lipid profile and reduce your risk.