Overview of Spine MRI
Magnetic resonance imaging (MRI) of the spine is a non-invasive diagnostic tool that utilizes a powerful magnetic field, radiofrequency pulses, and a computer to generate remarkably detailed images of the spine and its surrounding tissues. Unlike X-rays and CT scans, MRI does not involve the use of radiation, making it a safe and preferred option for many patients.
The high-resolution images produced by MRI allow doctors to examine the spine in exquisite detail, revealing abnormalities, injuries, and diseases that might not be visible with other imaging techniques. This makes MRI the most sensitive and informative imaging test currently available for evaluating the spine. While most MRI scans of the spine do not require contrast material, in some cases, a gadolinium-based contrast agent may be injected to enhance the visibility of specific tissues or abnormalities. Gadolinium is generally considered safe and less likely to cause allergic reactions compared to iodine-based contrast materials.
What are some common uses of the procedure?
MRI imaging of the spine is a versatile tool used to assess a wide range of conditions. It provides detailed anatomical views, allowing for the evaluation of spinal alignment and the detection of birth defects affecting the vertebrae or spinal cord. In cases of trauma, MRI can pinpoint injuries to the bones, discs, ligaments, or spinal cord itself, aiding in accurate diagnosis and treatment planning.
Moreover, MRI is instrumental in identifying disc and joint diseases, which are common culprits behind severe lower back pain and sciatica. It can also detect compression or inflammation of the spinal cord and nerves, shedding light on potential causes of neurological symptoms. Additionally, MRI plays a crucial role in diagnosing infections within the vertebrae, discs, spinal cord, or its protective coverings, known as meninges.
Tumors affecting the vertebrae, spinal cord, nerves, or surrounding soft tissues can also be identified and characterized using MRI, aiding in early detection and treatment planning. Beyond diagnosis, MRI guides surgical interventions such as decompression of pinched nerves and spinal fusion procedures. It also helps assess the effectiveness of steroid injections, often used for pain relief. By providing a comprehensive view of the spine's health, MRI enables ongoing monitoring of post-operative changes, such as scarring or infection, ensuring optimal recovery and long-term well-being.
How should I prepare for the Spine MRI?
Preparing for an MRI scan of the spine involves a few key steps. First, you'll be asked to change into a hospital gown to prevent any interference with the MRI's magnetic field and ensure your safety. While most medications can be taken as usual, guidelines regarding eating and drinking before the exam may vary depending on the specific procedure and facility, so it's important to follow your doctor's instructions.
Some MRI exams utilize a contrast material called gadolinium to enhance image clarity. If your exam requires contrast, you'll be asked about any allergies or health conditions like asthma, as well as any allergies to medications, food, or the environment. Gadolinium is generally safe and less likely to cause allergic reactions than iodine-based contrast, but your doctor will carefully assess your medical history before administering it.
Inform the technologist or radiologist about any serious health issues, such as kidney problems or recent surgeries, as these factors might influence the use of contrast or the overall safety of the procedure. If you have young children undergoing the scan, they might require sedation or anesthesia to remain still. The need for sedation depends on the child's age, developmental stage, and the type of exam. Pediatric sedation specialists are available at many facilities to ensure your child's safety and comfort.
Before entering the MRI room, remove all jewelry, accessories, and any metal or electronic items. These can interfere with the magnetic field, potentially causing damage to the device or posing a risk to you. This includes items like jewelry, watches, credit cards, hearing aids, hairpins, metal zippers, removable dental work, pens, pocketknives, eyeglasses, body piercings, and electronic devices like mobile phones and smartwatches.
While most metal implants are safe in an MRI environment, certain types, such as cochlear implants, aneurysm clips, metal coils in blood vessels, older cardiac devices, and vagal nerve stimulators, may pose risks. It's crucial to inform the technologist about any implanted medical or electronic devices you have, providing any relevant documentation to ensure safety during the scan. If there's any uncertainty, an X-ray can be used to identify metal objects.
If you have any shrapnel, bullets, or other metal fragments in your body, especially near the eyes, inform the medical staff. These can be hazardous due to potential movement or heating during the scan. While tattoo dyes containing iron might rarely cause issues, most dental fillings, braces, and cosmetics are generally safe, though they may affect image quality in the facial or brain areas. Finally, anyone accompanying you into the MRI room will also be screened for metal and electronic devices to maintain a safe environment.
What does the equipment look like?
The typical MRI machine resembles a large cylindrical tube enclosed by a circular magnet. During the scan, you'll lie on a movable table that slides into the center of this tunnel-like structure. However, variations exist to accommodate different patient needs and preferences. Some MRI units, known as short-bore systems, offer a more open design where the magnet doesn't completely surround you. Additionally, newer models often feature larger diameter bores, providing increased comfort for larger patients or those with claustrophobia.
Open MRI units, with their open sides, offer a less confined experience, making them particularly suitable for individuals who experience anxiety in enclosed spaces or those with larger body sizes. These open MRI units can still deliver high-quality images for various exams, but their applicability might be limited for certain specific procedures. If you have any concerns about the type of MRI unit best suited for your needs, it's advisable to discuss them with your radiologist, who can provide personalized recommendations and address any questions you may have.
How does the procedure work?
Unlike X-ray and computed tomography (CT) scans, which utilize ionizing radiation, MRI employs a powerful magnetic field and radio waves to generate detailed images of the body's internal structures. This non-invasive technique involves temporarily realigning the hydrogen atoms naturally present within the body, a process that doesn't cause any chemical alterations to the tissues. As these hydrogen atoms return to their normal state, they release varying amounts of energy, depending on the type of tissue they reside in.
The MRI scanner's coils, located both within the machine and sometimes placed around the specific body part being imaged, play a crucial role in transmitting and receiving radio waves. These radio waves interact with the hydrogen atoms, producing signals that are detected by the machine. Importantly, the electric current generating the magnetic field does not come into direct contact with the patient. A sophisticated computer then processes these signals, transforming them into a series of detailed cross-sectional images, each depicting a thin slice of the body. These images can be viewed from different angles, providing a comprehensive view of the internal structures. MRI's exceptional ability to differentiate between healthy and diseased tissue makes it a valuable diagnostic tool, often surpassing the capabilities of X-ray, CT, and ultrasound in certain cases.
How is the procedure performed?
MRI exams of the spine are typically outpatient procedures. You'll be positioned on a movable table, potentially with straps and bolsters for stability. Coils, which transmit and receive radio waves, might be placed around the specific area of your spine being examined. These exams usually involve multiple sequences, each with distinct sounds.
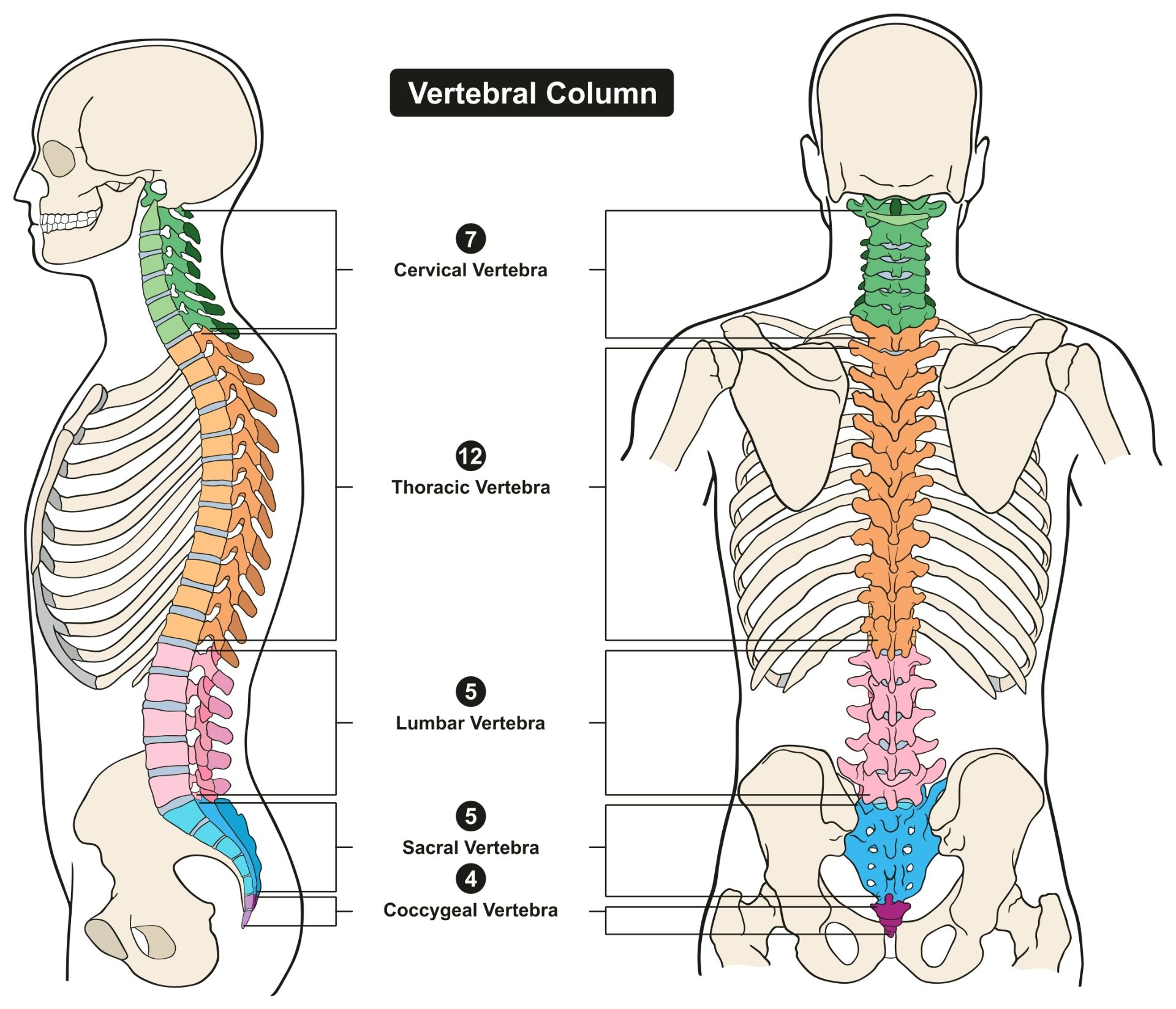
The area scanned depends on your symptoms; it could be the cervical (neck), thoracic (chest), or lumbar (lower) spine. If necessary, a contrast material called gadolinium might be injected via an IV to enhance image clarity. You'll lie inside the MRI machine, communicating with the technologist through an intercom. After the initial scans, you may briefly wait while the radiologist reviews the images.
Once finished, the IV (if used) is removed, and a dressing is applied. The exam usually takes 30-60 minutes, potentially longer if contrast is used.
What will I experience during and after the procedure?
While most MRI exams of the spine are painless, some individuals may find it challenging to remain still for extended periods. Additionally, the enclosed space within the MRI scanner can trigger claustrophobia in certain patients. The scanner itself generates noise, but earplugs or headphones are provided to minimize discomfort.
It's normal for the imaged area to feel slightly warm due to the radiofrequency pulses, and if this becomes bothersome, informing the technologist is recommended. Maintaining stillness is crucial for clear images, and you'll know when images are being recorded due to the loud tapping or thumping sounds from the activated coils. Although you may be able to relax between sequences, maintaining your position is essential.
Despite being alone in the exam room, you'll be under constant observation and in communication with the technologist through a two-way intercom. A "squeeze-ball" is provided for immediate assistance if needed. Some facilities allow a screened companion to stay with you during the scan for added comfort. Children receive appropriately sized earplugs or headphones, and music may be played to help them relax. MRI scanners are well-lit and air-conditioned to ensure a comfortable environment.
In certain cases, a contrast material may be injected intravenously (IV) before the scan to enhance image clarity. The IV needle might cause slight discomfort or bruising, and there's a minimal risk of skin irritation at the insertion site. Some patients experience a temporary metallic taste after the injection.
If you don't require sedation, you can typically resume your normal activities and diet immediately after the exam. Although rare, some individuals may experience side effects like nausea, headache, or pain at the injection site. Allergic reactions, such as hives or itchy eyes, are exceedingly uncommon, but if they occur, the technologist should be notified immediately, and medical assistance will be provided promptly.
Who interprets the results and how do I get them?
Following your MRI scan, a radiologist, a physician with specialized training in interpreting medical images, will meticulously analyze the images obtained during the procedure. The radiologist will then prepare a detailed report summarizing their findings and conclusions, which will be sent to your primary care physician or the doctor who referred you for the MRI. Your doctor will discuss the results with you, explaining any identified abnormalities or issues, and outline a plan for further evaluation or treatment if necessary.
In some cases, a follow-up MRI or additional imaging tests may be recommended. This could be to gain a deeper understanding of a potential problem, to monitor its progression over time, or to assess the effectiveness of any ongoing treatment. Follow-up exams are often a crucial step in ensuring accurate diagnosis and effective management of spinal conditions, providing valuable insights into the efficacy of interventions and guiding further decision-making.
Benefits
Magnetic Resonance Imaging (MRI) of the spine offers numerous advantages as a diagnostic tool. Notably, it's a non-invasive procedure that doesn't expose patients to harmful radiation. Compared to other imaging methods, MRI produces exceptionally clear and detailed images of the spine, revealing abnormalities, injuries, and diseases that might otherwise go undetected. It is particularly adept at visualizing the spinal cord and nerves, making it an invaluable tool for evaluating neurological conditions.
MRI's ability to penetrate bone and visualize structures that might be obscured in other imaging modalities further enhances its diagnostic value. Additionally, the gadolinium-based contrast material used in some MRI scans is less likely to trigger allergic reactions than the iodine-based contrasts used in X-rays and CT scans.
MRI's strengths extend to evaluating spinal injuries, where it can quickly diagnose or rule out acute spinal cord compression, especially when physical examinations indicate muscle weakness or paralysis. It is also the preferred method for assessing ligament injuries and detecting subtle changes in the vertebral column that might signal early signs of infection or tumors. Compared to CT scans, MRI is more sensitive in evaluating tumors, abscesses, and other soft tissue masses near the spinal cord. Moreover, it's the go-to method for assessing potential complications after spinal surgery, such as bleeding, scarring, infection, and the recurrence of herniated discs.
Risks
MRI scans of the spine are generally safe for most patients when safety guidelines are followed. However, it's important to be aware of potential risks. If sedation is used, there is a slight risk of administering too much, but this is minimized by closely monitoring vital signs.
The strong magnetic field used in MRI is harmless to most individuals, but it can interfere with the proper functioning of implanted medical devices or distort the images obtained. In rare cases, nephrogenic systemic fibrosis, a complication linked to gadolinium-based contrast agents, can occur, particularly in patients with severe kidney disease. Doctors carefully assess kidney function before considering contrast injections to mitigate this risk.
Although rare, allergic reactions to contrast material are possible, and these reactions are usually mild and easily managed with medication. Medical assistance is readily available in case of an allergic reaction. Recent studies have shown that trace amounts of gadolinium may remain in the body, especially the brain, after multiple MRI scans. This is more likely to occur in patients who undergo frequent MRI exams throughout their lifetime to monitor chronic conditions. Most of the contrast agent is eliminated through the kidneys, but if you fall into this category, discuss the possibility of gadolinium retention with your doctor, as it can vary from person to person.
For breastfeeding mothers, manufacturers of IV contrast advise against breastfeeding for 24-48 hours after receiving the contrast. However, the latest research from the American College of Radiology suggests that the amount of contrast absorbed by infants through breast milk is minimal. For further information and guidance, consult the ACR Manual on Contrast Media and its references.
What are the limitations of a Spine MRI?
While MRI is a powerful tool for diagnosing spinal conditions, it's important to be aware of its limitations. The quality of the images hinges on your ability to remain perfectly still and follow breath-holding instructions during the scan. If you're anxious, confused, or in severe pain, maintaining stillness can be challenging, potentially affecting image clarity.
Body size can also be a constraint, as some MRI machines have weight limits. Implants and other metallic objects, as well as patient movement, can interfere with obtaining clear images. An irregular heartbeat might also impact image quality in certain MRI techniques that rely on the heart's electrical activity for timing.
MRI is generally not recommended for critically injured patients due to potential interference from traction devices and life support equipment. However, medical professionals may still opt for MRI in certain trauma cases based on clinical judgment.
While non-contrast MRI is considered safe for pregnant women, doctors might postpone the scan until after delivery if it's not urgent. Gadolinium contrast agents are typically avoided during pregnancy unless absolutely necessary. Your doctor will discuss the benefits and risks of any MRI procedure with you, and MRI might be performed after the first trimester to assess fetal development when ultrasound findings are inconclusive.
Compared to other imaging exams, MRI tends to be more expensive and time-consuming. If you have concerns about the cost, it's advisable to consult with your insurance provider. In some cases, CT scans might be better suited for detecting vertebral fractures.