Overview of the Atherogenic Index of Plasma (AIP)
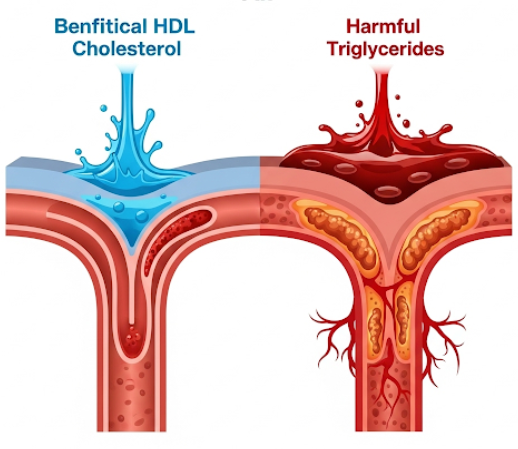
The Atherogenic Index of Plasma (AIP) is a comprehensive biomarker utilized to assess an individual's inherent risk for developing cardiovascular disease. This index is derived through a straightforward calculation that incorporates two critical components from a standard lipid panel: triglycerides (TG) and high-density lipoprotein cholesterol (HDL-C). Specifically, the AIP is determined by taking the base-10 logarithm of the ratio between the triglyceride concentration and the HDL-C concentration, expressed as: AIP = log10 (Triglycerides / HDL-C). Introduced by Dobiasova and Frohlich in 2001, the AIP has since gained significant recognition for its sensitivity and robust capability in reflecting the crucial balance between lipoproteins that either promote or prevent the formation of atherosclerotic plaque within arteries. A pivotal aspect of AIP's diagnostic utility lies in its direct correlation with the size of lipoprotein particles, particularly the presence of small, dense LDL particles, which are known to be highly atherogenic. By integrating the levels of both triglycerides and HDL-C, the AIP offers a more holistic and nuanced perspective on dyslipidemia and an individual's overall cardiovascular risk profile, surpassing the insights gained from analyzing individual lipid parameters in isolation. Consequently, it serves as an accessible and highly valuable metric for evaluating the likelihood of atherosclerosis development and for effectively monitoring the efficacy of various lipid-modifying therapeutic interventions and lifestyle adjustments.
Why the Atherogenic Index of Plasma is Done
The Atherogenic Index of Plasma (AIP) is increasingly employed as a valuable tool in both the assessment and proactive management of cardiovascular risk. Healthcare providers primarily request an AIP calculation to gain a more precise and encompassing understanding of an individual's predisposition to developing atherosclerosis and subsequent cardiovascular diseases, including but not limited to coronary artery disease, myocardial infarction (heart attack), and cerebrovascular accident (stroke). While traditional lipid markers, such as LDL and HDL cholesterol levels, certainly offer important diagnostic information, the AIP provides enhanced predictive value. It achieves this by reflecting the intricate and often nuanced interplay between triglycerides and HDL-C, a relationship that is strongly associated with lipoprotein particle size and the overall burden of atherogenic lipids. The AIP proves particularly useful in identifying individuals who may be at an unexpectedly elevated risk, even if their conventional lipid profiles appear to fall within normal or near-normal ranges. For example, a characteristic pattern of atherogenic dyslipidemia often involves high triglyceride levels coupled with low HDL-C levels, and the AIP effectively encapsulates and highlights this specific imbalance. Furthermore, the AIP serves a crucial role in monitoring the effectiveness of various therapeutic interventions. These interventions can range from fundamental lifestyle modifications, such as targeted dietary changes and increased physical activity, to the administration of specific lipid-lowering medications. By monitoring changes in AIP values, clinicians can more effectively tailor and refine treatment strategies, ultimately aiming to optimize patient outcomes and significantly reduce the likelihood of adverse cardiovascular events. The index acts as a robust biomarker for screening diverse populations, especially those with recognized risk factors such as obesity, diabetes mellitus, and metabolic syndrome, thereby facilitating early detection and fostering proactive approaches to cardiovascular disease prevention.
Risks
The Atherogenic Index of Plasma (AIP) itself is not a direct procedure but rather a calculated value derived from a standard blood test, specifically a lipid panel. Consequently, any risks associated with obtaining the AIP are those inherently linked to a routine blood draw, which is medically termed venipuncture. These risks are generally considered minimal, typically temporary in nature, and localized to the site of the blood collection. Common, minor side effects that an individual might experience include a slight, brief pain or a transient stinging sensation precisely at the moment the needle is inserted into the vein, most often in the inner elbow region of the arm. Following the successful collection of the blood sample, it is quite common for a small bruise to form at the puncture site; however, such bruising usually resolves spontaneously within a few days without necessitating any specific medical intervention. In some rarer instances, individuals may experience mild dizziness or a sensation of lightheadedness, particularly if they have a known history of feeling faint during blood drawing procedures. Very uncommon complications include the formation of a hematoma, which is a localized collection of blood under the skin, should bleeding persist internally at the puncture site. Furthermore, the risk of developing an infection at the site of puncture is exceedingly low, provided that strict sterile techniques are rigorously followed by the healthcare professional performing the venipuncture. For individuals who are currently taking anticoagulant, or blood-thinning, medications, there might be a slightly increased propensity for bleeding or bruising; this should always be clearly communicated to the phlebotomist prior to the commencement of the procedure. Overall, the blood collection process required for the lipid panel, from which the AIP is calculated, is widely regarded as a very safe diagnostic procedure that carries negligible long-term health risks for the vast majority of patients.
How You Prepare
Proper and meticulous preparation for the blood test necessary to calculate the Atherogenic Index of Plasma (AIP) is absolutely essential to guarantee the accuracy and reliability of the resulting values. Since the AIP is mathematically derived from an individual's triglyceride and HDL-cholesterol levels, the preparatory guidelines are identical to those mandated for a standard fasting lipid panel. The most critical instruction for preparation involves a mandatory fasting period of 9 to 12 hours before the scheduled blood sample collection. During this designated fasting window, individuals must strictly refrain from consuming any food or drinks, with the sole exception of plain water. This rigorous fasting requirement is paramount because recent food intake, especially meals that are high in fat content, can significantly and artificially elevate triglyceride levels, which directly impacts the accuracy of the subsequent AIP calculation. Furthermore, it is highly recommended and often a strict instruction to avoid all alcohol consumption for at least 24 hours prior to the test, as even moderate alcohol intake can substantially raise triglyceride levels. You are also obliged to inform your healthcare provider about all medications you are currently taking, encompassing prescription drugs, any over-the-counter medications, vitamins, and herbal supplements. Certain medications are known to influence lipid levels, and your doctor may, in specific circumstances, advise you to temporarily adjust or discontinue some of them before the test. However, it is crucial to emphasize that you must never alter your prescribed medication regimen without explicit and direct instruction from your doctor. Additionally, engaging in strenuous physical activity immediately preceding the test should also be avoided, as intense exertion can temporarily affect lipid levels. Adhering diligently to these specific preparation guidelines provided by your healthcare provider is key to ensuring that your lipid profile, and consequently your AIP, accurately reflects your true and typical metabolic state.
What You Can Expect
Before the Test
Before your scheduled blood test for the Atherogenic Index of Plasma (AIP), your primary responsibility will be to meticulously adhere to any preparatory instructions provided by your healthcare provider. A common and crucial directive for this test involves fasting for a period of 9 to 12 hours prior to the blood draw, during which only plain water is permitted for consumption. This fasting requirement is absolutely essential because triglyceride levels, which are a fundamental component of the AIP calculation, are highly sensitive to and can be significantly influenced by recent dietary intake. Furthermore, it is imperative that you avoid all alcohol consumption for a minimum of 24 hours (or potentially longer, if specifically instructed) before the test. This strict avoidance is due to alcohol's potent capacity to substantially elevate triglyceride levels, directly affecting the accuracy of the estimated VLDL component and thus the AIP. You must also comprehensively inform your doctor about all prescription medications, over-the-counter drugs, herbal remedies, and any dietary supplements you are currently taking, as numerous substances can influence lipid levels. Your doctor may, after reviewing your medical history and current medications, advise you to temporarily discontinue or adjust certain ones. However, any such changes must only be made under their direct medical guidance. Additionally, it is generally advisable to refrain from strenuous physical activity just before the test, as intense exercise can also temporarily alter lipid values. Arriving at the clinic or laboratory feeling calm, relaxed, and adequately hydrated will contribute to a smoother blood collection process. If you tend to experience anxiety or discomfort related to blood draws, communicating this to the phlebotomist beforehand can be helpful, as they can employ techniques to make the experience more comfortable for you. These careful preparatory steps are vital for ensuring the integrity and accuracy of your test results, ultimately helping to ensure that the blood sample collected genuinely reflects your true lipid levels for appropriate clinical interpretation.
During the Test
During the blood collection for the Atherogenic Index of Plasma (AIP), you will undergo a procedure that is virtually identical to any other routine blood test. You will typically be asked to sit comfortably, usually in a specialized chair designed for blood draws, which allows the healthcare professional easy access to your arm. A trained and qualified healthcare professional, such as a phlebotomist or a nurse, will carefully examine your arm to identify a suitable vein for drawing the blood. The most common site for this procedure is the inside of your elbow, often referred to as the antecubital fossa, although sometimes a vein on the back of your hand may be utilized. Before inserting the needle, the selected area of skin will be meticulously cleansed with an antiseptic wipe. This crucial step is performed to maintain rigorous sterility and effectively minimize any potential risk of infection at the puncture site. To make the chosen vein more visible and prominent, and thus easier to access with the needle, a tourniquet may be gently tied around your upper arm. This temporary measure increases blood flow to the vein, causing it to swell slightly. Once the vein is adequately prepared, a sterile, single-use needle will be carefully inserted. At this point, you are likely to experience a brief, sharp prick or a mild stinging sensation as the needle penetrates the skin. Blood will then steadily flow into one or more small, designated collection tubes. The actual process of blood collection is remarkably swift, typically concluding within just a few minutes. After the necessary amount of blood has been obtained, the tourniquet will be released, and the needle will be smoothly withdrawn from your arm. Immediate pressure will then be applied to the puncture site using a clean cotton ball or gauze, a step vital for stopping any bleeding and minimizing the formation of bruising.
Results
After your blood sample for the Atherogenic Index of Plasma (AIP) is meticulously collected, it will be promptly transported to a medical laboratory for comprehensive analysis. Within the laboratory, specialized technologists will accurately measure the concentrations of both triglycerides and high-density lipoprotein cholesterol (HDL-C). Once these critical lipid values are precisely determined, the Atherogenic Index of Plasma will be mathematically calculated using its specific formula: log10 (Triglycerides / HDL-C). The resulting AIP value, typically expressed as a numerical figure, will then be securely transmitted to your healthcare provider, generally within a few days. Your doctor will undertake the crucial task of interpreting your individual AIP value by comparing it against established reference ranges. It is important to note that while specific ranges may exhibit slight variations between different laboratories, broad guidelines for AIP interpretation are widely accepted in clinical practice. For instance, AIP values typically less than 0.11 are generally associated with a low risk of cardiovascular disease. Values falling between 0.11 and 0.21 commonly indicate an intermediate risk. Conversely, AIP values greater than 0.21 are generally associated with a significantly increased risk of developing cardiovascular disease. Your doctor will thoroughly discuss your AIP result with you, providing a clear explanation of what it signifies for your overall cardiovascular health. They will consider this result in conjunction with your complete medical history, other components of your lipid panel, relevant lifestyle factors, and any other pertinent clinical information to formulate a personalized assessment of your cardiovascular risk. Based on this comprehensive evaluation, your doctor will then recommend appropriate management strategies. These may encompass targeted lifestyle modifications, such as specific dietary changes and increased physical activity, or, if deemed necessary, pharmacological interventions designed to optimize your lipid profile and effectively reduce your overall cardiovascular risk, thereby promoting long-term heart health.